Co-designing, implementing and evaluating a patient navigation model of care to meet the complex needs of NT youth presenting to the Emergency Department.
Young people in the Northern Territory (NT) are twice as likely to be at risk of alcohol related harm, three times more likely to be admitted to hospital for assault and injuries and are disproportionately represented in the criminal justice and child protection system (NTG, 2018b). In 2017, young people aged 15-24 in the NT had a death rate of 106.3 per 100,000 (ABS, 2017). This is three times the national rate, with the majority of deaths being due to causes that are considered largely preventable in the current health system (Vincentiis et al, 2019). Reflecting these high rates of mortality and morbidity, young people in the NT access hospital services more frequently than in any other Australian jurisdiction (AIHW, 2019). The NT has the highest overall rate of emergency department presentations among those aged 10-19 in Australia, and the highest hospitalisation rate for Indigenous young people aged 10-24 (196 per 1000) (AIHW, 2018). The rate of ED re-presentation within 28 days for patients in the NT aged 15-24 is 22% (unpublished NT data) compared to 18.4% nationally (AIHW, 2018).
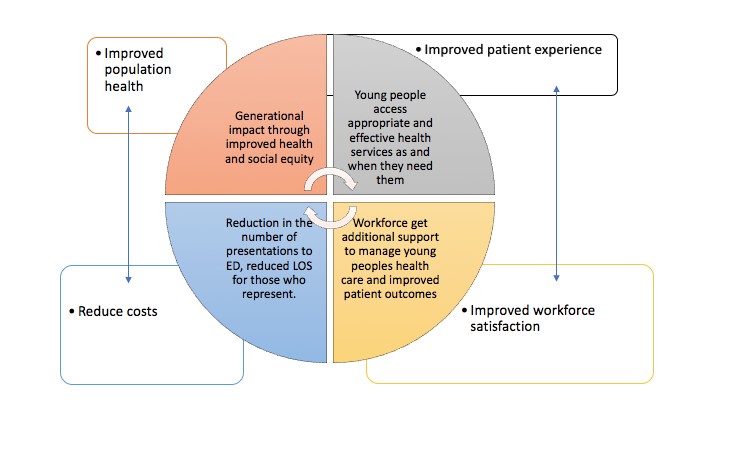
Young people often present to ED in crisis and have complex environmental and social concerns which are multidimensional and span across sectors: education, housing, child protection and mental health services. Delivering care to meet these needs is often complex and requires a range of interventions. Despite the known disparities and frequent interactions with the hospital system, there is no model of care within the ED that specifically addresses the needs of the youth population. Whilst there are many complex determinants to adolescent health outcomes there are significant opportunities to address both health and social needs within the acute system. There is strong emerging evidence of the positive impact of patient navigator models both internationally and in Australia (World Health Organization, 2022). It is increasingly recognised as an essential model of care for patients with repeat emergency presentations and within acute settings and is particularly beneficial for transitional care groups and populations who experience disadvantage and barriers to services (WHO, 2022).
An important component of this model of care will be accurate assessment and identification of risk and protective factors, safety planning and referral to community services. Support will be provided to young people who have been identified as having significant risk factors and complex needs for 6-8 weeks to ensure they are engaged with important community services.
This project will aim to meet the needs of adolescents in the NT and improve health equity through Participatory Action research. It will co-design, implement and evaluate a model of care for adolescents who access the ED at Royal Darwin Hospital, with a focus on assessing risk, addressing social determinants and engaging young people with community supports and reducing the burden on the acute system through reduced representations and other hospital avoidance measures.
Project Aims:
- To understand how we can address the needs of adolescents accessing the acute care system through co-design with young people, and consultation with the workforce and community providers. These findings will be used to design the model and to create KPI’s and evaluation methods based on patient and workforce values.
- To understand the health and social and emotional wellbeing needs of young people through health and psychosocial screening (data to be collected on health, comorbidities, psychosocial factors and hospital presentation data).
- To work towards a model of integrated care by referring young people to appropriate community supports and provide short term navigation until the young person has engaged. (identified through screening).
- Assess hospital avoidance data to measure impact of the model and evaluate its success alongside a health economist.
Key staff:
- Marita Hefler
- Rachel Buckley